Old and new serum therapy
Serum Therapy of Shibasaburo Kitasato
and Modern Serum Therapy
- Shibasaburo Kitazato Museam
- Directo Hidero Kitasato
- St. Luke’s International Hospital, Department of Emergency and Critical Care Medicine
- Chief of Staff Toru Hifumi
Serum therapy was first used in the world in 1889 by Dr. Shibasaburo Kitasato, who was studying under Dr. Robert Koch in Berlin, Germany, in “On the Establishment of Diphtheria and Tetanus Immunity in Animals,” using tetanus toxin1. The publication date of that article, December 4, is considered Serum Therapy Day in Japan (Figure 1). This paper marked the moment when mankind had its first effective means against infectious diseases, revealing the existence of antibodies (antitoxins) and at the same time allowing them to be used in other animals, including other humans. Today, serum therapy is mainly used for snake venom, but this paper looks back at the history of serum therapy.
First human serum therapy by Dr. Shibasaburo Kitasato
Animals injected with a pure culture of tetanus bacillus develop typical tetanus, but since the bacillus is not detected except locally, we assumed that it is caused by toxins and devised and certified a bacterial filtration machine. Next, we found that this toxin was destroyed by iodine trichloride solution, which, when used in combination with a small amount of tetanus culture medium in increments and injected repeatedly into rabbits, enabled them to tolerate injections of the culture medium containing the potent toxin and tetanus spores. Animal experiments and in vitro neutralization experiments have discovered the presence of antitoxins or antibodies that detoxify the toxin in rabbit serum. The serum was also effective in other animals, indicating the possibility of a new treatment. Dtsch.med. Wschr. 16:1113-14, 1890 (Figure1).1
A summary of the paper is as follows:
- Blood or serum from rabbits that have become immune to tetanus destroys the tetanus toxin in vitro.
- This serum shows similar efficacy in mice.
- Hence, rabbit sera that have become immune to tetanus can be applied to the prevention or treatment of tetanus.
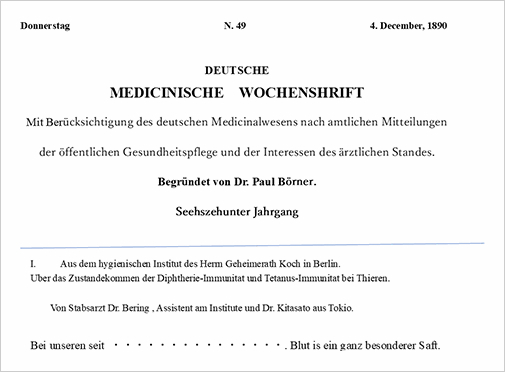
This paper proposed a new immune mechanism and treatment for toxin-type infections such as diphtheria and tetanus for the first time in the world. The paper closes with the following words from Goethe: Blut ist ein ganz besonder Saft (Blood is a very special liquid)
Diphtheria Serum Therapy in Japan by Dr. Shibasaburo Kitasato
The diphtheria serum therapy began in August 1893 with the immunization of sheep purchased in July 1893, and serum was collected in November of the following year and used on diphtheria patients hospitalized at the Institute for Infectious Diseases that year, with remarkable results. The cooperation of veterinarian Shinkichi Umeno was indispensable. In this method,2 the horse was injected with one-thousandth or one-ten-thousandth of the lethal dose of diphtheria culture inactivated by carbolic acid or other means, and the dose was increased for a time. Doses were increased after 12 days, with an interval of 5-10 days depending on the condition of the animals. Finally, the bacteria were injected at several hundred to a thousand times the lethal dose, and those that tolerated the injections were deemed to have reached advanced immunity. It was assumed that a large amount of antitoxin was present in this animal serum. First, 2500 ml of blood was collected with a sterile glass syringe and needle three times every other day. The blood collected in the glass cylinder coagulated and deposited serum in the upper layer of the vessel, which was divided into blood clots. To this serum, carbolic acid was added for antiseptic purposes at 0.5% to make a treatment serum.
The treatment serum confirmed the following:2,3
- Serum effects were tested.
- Sterility of serum (sterility by aerobic or anaerobic culture) was confirmed.
- No presence of toxic substances in the serum (5 ml were injected into guinea pigs to confirm that it is harmless).
- Carbonic acid did not dilute above 0.5% (0.5 ml were injected into rats to confirm that it is harmless).
- Protein content was not higher than 10% protein (determined by the Kjeldahl nitrogen determination method).
The Effects of Serum Therapy
- Regarding the time from infection to the serum injection
- Serum usage
- Dependence on the method of serum injection
- Results of diphtheria serum therapy (1895)3,4
1. Regarding the time from infection to the serum injection
In the animal experiments of Dönitz Berghaus, it was found that after two hours, the amount of antitoxin was ten times greater than at one hour, and after six hours, however large the amount of antitoxin that could be neutralized, no amount of antitoxin could save the patient from death.
2. Serum usage
The therapeutic dose of serum required for the treatment should be determined according to clinical observations. Unlike other drugs, serum is not harmful even when used in large quantities, and its efficacy is high. Hence, it was recommended to use a great deal of serum at once, as early as possible. Contrary to this, the initial use of a small amount was felt to be insufficient afterwards, and further repeated injections were less effective than the initial use of a larger amount.
3. Dependence on the method of serum injection
Subcutaneous injections were absorbed slower, muscle injections somewhat faster, and intravenous injections the fastest (according to Berghaus’ experiments, muscle injections are 5 to 7 times more effective than subcutaneous injections, and intravenous injections are 500 times more effective).
4. Results of diphtheria serum therapy (1895)3,4
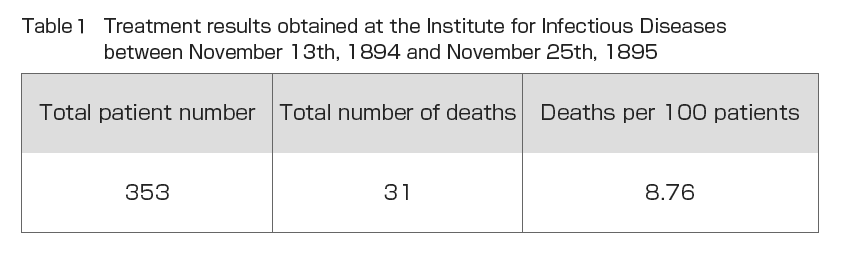
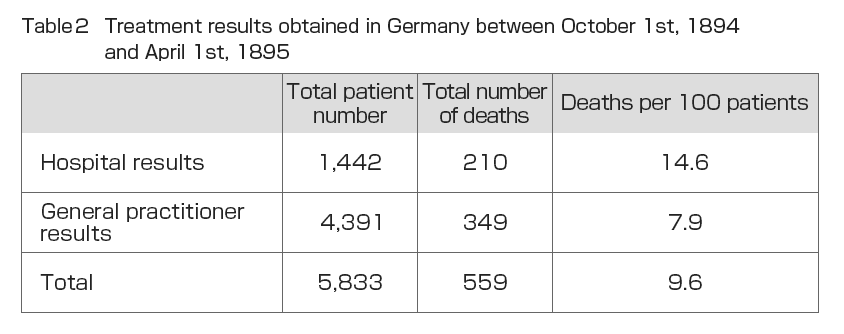
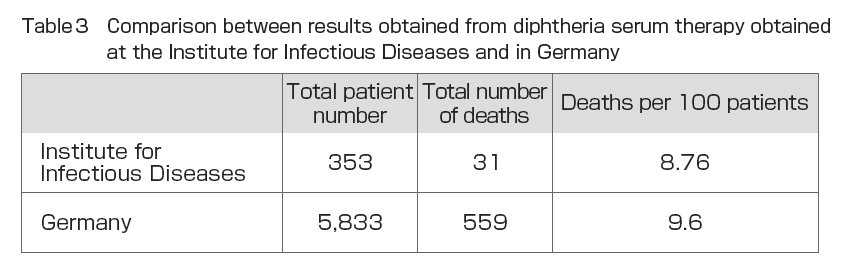
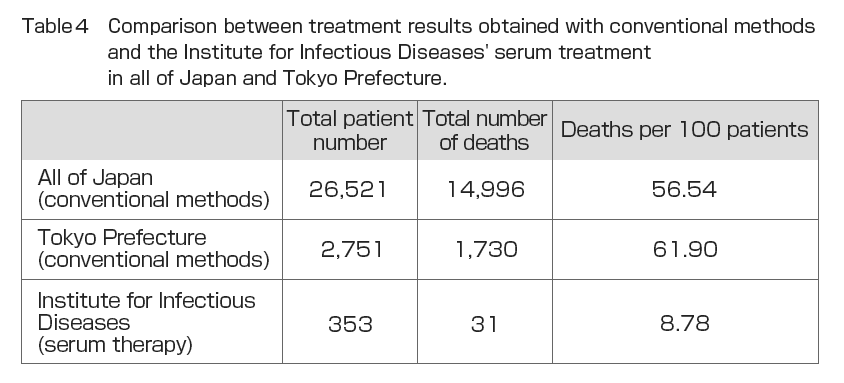
During his time at the Institute for Infectious Diseases, Dr. Shibasaburo Kitasato conducted experiments in 1895 on the treatment of humans using serum made from horses and other animals at the Serum Institute of the Imperial Government of Japan with the cooperation of veterinarian Shinkichi Umeno and others (Fig. 2). The treatment consisted of injecting 10 and 20 ml of serum into the patient, with an interval of one or two hours when larger doses were required. In emergencies, injections were continued as appropriate. The injection site was injected subcutaneously on the thoracic side or inside the thigh. The injection site was washed and sterilized, and after injection, a drop of 5% “collodium” iodine solution was dropped into the needle scar area without rubbing the area and allowed to clot. From November 13, 1894 to November 25, 1895, a total of 356 diphtheria patients were treated with serum and 31 died. Of the total number of patients, three patients had pseudomembranes in the pharynx and a fever that should have been clinically diagnosed as diphtheria, but no diphtheria was detected on bacteriological examination. These patients were excluded from the total number of patients (). also shows the results of diphtheria serum therapy in Germany between October 1, 1894 and April 1, 1895, as reported by Behring. The mortality rate per 100 patients was 14.6 for hospitals and 7.9 for general practitioners, suggesting that the reason why general practitioners have a better treatment outcome may be that they have more opportunities to see patients in the early stages of the disease and can start serum therapy immediately. compares these results with the results of the Institute for Infectious Diseases. The mortality rate of 8.76 deaths per 100 patients at the Institute for Infectious Diseases hospital was almost the same as the total of 9.6 for the German hospitals plus general practitioners, and 5.82 higher than the 14.6 for the German hospitals. The results were also compared with those of seven years of treatment between 1888 and 1894 in Japan by conventional methods (Annual Report of the Bureau of Public Health) (). The results showed that serum therapy improved mortality by 47.76%. Similarly, a 53.12% reduction in mortality was observed when compared to conventional treatment methods in Tokyo Prefecture ().
Serum treatment had no deaths if the start date was within two days of illness onset, and the longer it took, the worse the outcome. This is because the diphtheria antitoxin in the patient’s blood neutralizes the toxin but does not act to recover the organic changes in the peripheral nerves already caused by the diphtheria toxin. Therefore, it states that serum therapy should be initiated as soon as possible after the onset of the disease in order to ensure its success.
Figure2-1

Purchasing sheep for diphtheria serum no. 1 in July 1893. From August the sheep were immunized against diphtheria, and from the November of the following year, serum was extracted and the effects were confirmed for the first time in diphtheria patients hospitalized at the Institute for Infectious Diseases.
Figure2-2

Manufacturing sera for diphtheria and other types of diseases, it has been operated by the state since its establishment in 1896 as a place for students of Shibasaburo from the then Institute for Infectious Diseases, Japan Private Hygiene Society.
Also, as a branch adjacent to the Tsukushigaoka Yojoen tuberculosis hospital in Shirogane, serum was made using horses and sheep.
Images provided by the Kitasato Institute
Modern Serum Therapy
- Antivenom (antitoxin) preparations
- Fundamental approach to serum therapy
- Serum therapy in practice (route of administration)
- Effects of Serum Therapy
- Side effects of serum therapy
1. Antivenom (antitoxin) preparations
The production process is basically the same as that of Dr. Shibasaburo Kitasato’s therapeutic serum production even today, where horses are immunized and their blood is collected. In modern times, equine immunoglobulin is further purified from the obtained serum or plasma, then filled into vials and formulated as a lyophilized drug product.5 The fact that the serum was formulated differs from Dr. Shibasaburo Kitasato’s therapeutic serum, and it can be inferred that the administration of therapeutic serum at that time was similar to “blood transfusion therapy” in modern clinical medicine. In modern times, for example, quality control tests are conducted every year for Yamakagashi antitoxin used in clinical research, and titer tests are conducted once every few years to ensure that the quality of the product meets certain standards.
2. Fundamental approach to serum therapy
After a certain period of time, no amount of antitoxins, no matter how massive, can prevent death.
Antitoxin takes the neutralization of free toxins in the blood as the pathophysiological principle of its effect. Therefore, it is still considered today that it is difficult to anticipate the effect of a large amount of antitoxin when the toxin has already bound to its receptor and caused symptoms after a certain period of time. However, in cases such as a Yamakagashi bite, even if the patient has been bleeding for several days, the symptoms improve with administration of Yamakagashi antitoxin,6 and therefore, treatment with serum therapy should not be given up just because some time has elapsed.
3. Serum therapy in practice (route of administration)
Dr. Shibasaburo Kitasato’s therapeutic serum was administered intravenously or subcutaneously. Although subcutaneous, intramuscular, and intravenous administration of antitoxins are all recommended in modern literature, we recommend intravenous administration (intravenous infusion).5 The main reason for this is that not only is an immediate effect expected, but also the fact that securing an intravenous route means that the drug can be used as a route of administration in an emergency, which is of great significance in clinical settings, such as when dealing with anaphylaxis. In prehospital settings, such as at the beach or in the mountains, intramuscular injection may be considered when it is the only available option.
4. Effects of Serum Therapy
Dr. Shibasaburo Kitasato’s therapeutic serum dramatically improved the mortality rate from diphtheria at that time. Nowadays, with the progress of vaccination, diphtheria patients are rarely encountered in Japan, and it is difficult to compare the effects directly.
Antivenom is firmly established as a curative treatment for Yamakagashi bites, as there have been no deaths in cases in which Yamakagashi bites have been (or could have been) treated with antivenom.6 Serum therapy has also been initiated for Clostridium perfringens sepsis with hemolysis, currently one of the most lethal infectious diseases. This is caused by alpha toxin from C. perfringens, which rapidly leads to intravascular hemolysis, severe anemia, disseminated intravascular coagulation syndrome, and multiple organ failure, resulting in death.7 Van Bunderen et al. reported a series of cases of intravascular hemolysis due to C. perfringens sepsis that resulted in death within hours, with a mortality rate exceeding 80%.8 Although administration of antimicrobial agents and drainage of infected lesions are the main principles of treatment, in addition to this, the use of a neutralizing antibody against alpha toxin — gas gangrene antitoxin — the main virulence factor of C. perfringens [Clostridium perfringens (C. perfringens Type A, Clostridium septicum, and Clostridium oedematiens), an antitoxin manufactured against it (a national stockpile of insurance-approved drugs that can be used against this disease)], began to be considered for administration due to its pathology, and as of 2023, a prospective observational study of the administration of gas gangrene antitoxin for C. perfringens sepsis has already begun.
5. Side effects of serum therapy
According to Dr. Shibasaburo Kitasato’s Diphtheria and Cholera Morbus Outcome Report,4 there are scattered reports of the appearance of an urticaria-like skin rash a few days after administration of the serum.4 It is assumed it means urticaria in English. In 2022, we observed a similar itchy skin rash after 1 week of treatment with antitoxin in a patient with a severe case of a Yamakagashi bite, which may have been a similar immune response.
The description of what appears to be anaphylactic shock immediately after administration of the serum, which is of great concern today, was not clearly identified in the Diphtheria and Cholera Morbus Outcome Report4.
Summary
“The striking examples of Yamakagashi antitoxin’s application
made a strong impression of the effects of serum therapy.”
“The gas gangrene antitoxin used against
C. perfringens septicemia shines a light of hope into the future.”
Dr. Shibasaburo Kitasato openly denied the “tetanus culture symbiosis theory” that only tetanus bacilli could not be cultured in pure form at a seminar in the Koch laboratory, and despite the cynicism of those around him, through tireless efforts and a belief in practical science, he developed a turtle-shaped petri dish (Kitasato-type flask), replaced oxygen with hydrogen using Kipp’s aparatus, and conducted precise repeated experiments. Finally, in 1889, he succeeded in pure culture of the tetanus bacillus.9 He discovered that tetanus toxin causes tetanus10 and established serum therapy using animals immunized with the toxin, ultimately saving many lives from diphtheria, tetanus, and other infectious diseases caused by the toxin. As for Dr. Shibasaburo Kitasato’s serum therapy, his mentor, Robert Koch, later said: “When I heard intimately about the method and sequence in which Kitasato obtained the pure culture of tetanus, I was amazed at his extraordinary research mind and indefatigable spirit. He continued his research on tetanus toxin and finally produced an immune serum. At that time, there was still no single causative therapy for infectious diseases, and indeed, Kitasato’s research led to the creation of serum therapy.11,12 Diphtheria and tetanus are now rarely seen in Japan due to vaccines, but serum therapy still saves many lives from snake venom. The dramatic recovery from Yamakagashi bites with the administration of the antitoxin has strongly impressed us with the efficacy of serum therapy, and the treatment of C. perfringens sepsis with the gas gangrene antitoxin has given us hope for the future of serum therapy.
References
- Behring E & Kitasato S. Dtsch. med. Wschr., 49:1113-14, 1890.
- Serum Vaccine Usage Guidelines Kitasato Institute, Bacteriological Journal, 1936
- Shibasaburo Kitasato – My Mission to Control Infectious Diseases, The Kitasato Institute Kitasato Memorial Museum
- Editorial: Diphtheria and Cholera Morbus Outcome Report, Shibasaburo Kitasato, Director of the Institute for Infectious Diseases, Journal of Bacteriology, No. 1
- Toru Hifumi. Serum Therapy. Journal of the Japanese Society of Intensive Care Medicine 2018;25:235-42.
- Hifumi T, Sakai A, Yamamoto A, Murakawa M, Ato M, Shibayama K, Kato H, Koido Y, Inoue J, Abe Y, Kawakita K, Hagiike M, Ginnaga A, Kuroda Y. Effect of antivenom therapy of Rhabdophis tigrinus (Yamakagashi snake) bites. J Intensive Care. 2014 Jul 31;2(1):44
- Hifumi T. Spontaneous Non-Traumatic Clostridium perfringens Sepsis. Jpn J Infect Dis 2020;73:177-80.
- van Bunderen CC, Bomers MK, Wesdorp E, et al. Clostridium perfringensepticaemia with massive intravascular haemolysis: a case report and review of the literature. Neth J Med 2010;68:343-6.
- Kitasato、S. Ueber den Tetanusbacillus. Z. Hyg., 7, 225-234, 1989.
- Kitasato S. Experimentelle Untersuchungen über das Tetanusgift. Z Hyg., 10, 267-305, 1891.
- A Memory of Koch’s Visit to Japan. Shiga, Kiyoshi Recollections of a Bacteriologist, Sekkasha, 1966.
- Shibasaburo Kitasato Akihiro Ueyama
PROFILE
St. Luke’s International Hospital, Department of Emergency and Critical Care Medicine, Chief of staff of CCM, HCU
Toru Hifumi
The only person nationwide involved practice and research of serum therapy, bringing Dr. Shibasaburo Kitasato’s serum therapy into the present. While active as an on-site emergency physician of critical care, day and night, he dedicates himself to the research of venomous creatures. For 24 hours a day, 365 days a week, he is in charge of severe cases throughout Japan as a part of clinical research that uses Yamakagashi antivenom. His areas of expertise are serum therapy, neurological intensive care, trauma, sepsis, and airway management.
Shibasato Kitazato Museum, Director/Kitasato University, Professor Emeritus
Hidero Kitasato
The great-grandson of Shibasaburo Kitasato, the bacteriologist immortalized in the history of medicine by establishing serum therapy. Having experience as an overseas researcher himself, after becoming professor and head of the School of Allied Health Sciences at Kitasato University, he retired to the Kitazato Memorial Museum in July 2022, where he remains to date.